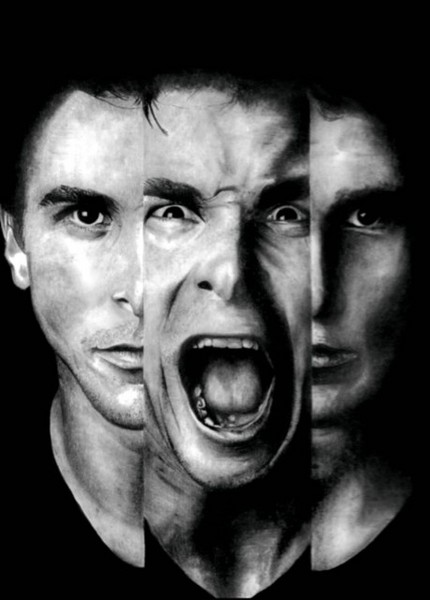
The schizophrenia is a group of disorders manifested by characteristic alterations of mood and behavior.
The main types are:
- Simple: It is characterized by a slow and insidious loss of volition, ambition and interest, which gives rise to deterioration of mental processes and interpersonal relationships and adjustment to a lower level of functioning.
- Hebephrenic. Characterized by disorganized thinking, lack of affection and inappropriate, idiotic and mannerism, often involves hypochondriacal manifestations.
- Catatonic
- Variety excitedly characterized by excessive motor activity and excitement and sometimes violent;
- Inhibited characterized by generalized inhibition behaviorally revealed by stupor, mutism, negativism and waxy flexibility.
- Schizoaffective. Is characterized by a mixture ratio or schizophrenic symptoms and severe depression. Paranoid. It is characterized by delusions of persecution or grandeur, hallucinations, sometimes excessive religiosity, and hostile or aggressive behavior.
- Chronic undifferentiated. mixed schizophrenic Symptoms (or other types), along with alterations of thought, affect and behavior.
Causes of Schizophrenia:
About 1% of Americans suffer from schizophrenia so programs are required to create awareness about the importance of nursing diagnosis for schizophrenia, are required. Such programs would enable public to know the causes of schizophrenia and process of nursing diagnosis for schizophrenia will become easy. Moreover, fewer cases of this illness will emerge out. Some main causes of schizophrenia involve:
- Environmental factors- social factors are largely responsible in causing schizophrenia as it is a psychosocial disorder. Traumatic events in life, poor relationship and sudden disastrous changes play an important role in onset of this illness. Patient becomes paranoid and fear anything new coming in his life. He becomes unable to cope with the physical or environmental changes and stress, and anxiety occurs. Hostile or critical parentage can also increase the risk of schizophrenia. Urbane lifestyle also increases the chances of schizophrenia.
- Genetic factors also contribute to the risk of onset of schizophrenia. Many genes are responsible for it making it a complex illness. During nursing diagnosis for schizophrenia, family histories are considered as major factors.
- Misuse of certain substances is reported to cause schizophrenia. Alcohol, cannabis, nicotine and various other substances are involved in it.
The prognosis:
- when the patient has a history of good social adjustment, and sexual labor.
- when the onset of the disease is acute.
- if there was a triggering event. Note that patient probably also was taking medications such as tranquilizers or antipsychotics.
Behaviors or problems:
- Conduct withdrawn or inhibited.
- Regressive behavior.
- Increased anxiety, agitation
- Decreased self-esteem.
- Loss of the limits of self-inability to perceive or distinguish the self-concept of the elements of the external environment
- Hallucinations
- Delusions
- Disorganized thinking, illogical
- Inadequate or insufficient emotional responses
- Disorders of volition and goal-directed activity
- Bad relationships
- Difficulty engaging verbal communication
- Exaggeration (le responses to stimuli
- Aggression toward self, others or property
- Sleep disturbances, fatigue
- Eating disorders, poor nutrition
- Sexual conflicts
- Constipation
- Menstrual disorders
SHORT TERM GOALS
- Nutrition sufficient regularity emunctories, adequate rest and safe activity.
- Keep the patient in a safe environment.
- Establish communication and build trust. Helping the patient to participate in the therapeutic community.
- Increase the patient’s ability to communicate with others.
- Decrease of hallucinations, delusions and other psychotic symptoms.
- Reduce injury or pulse action.
- Increase self-esteem.
LONG TERM GOALS
- Identify and use the forces and potentialities, and develop a better self-image.
- Achieve and maintain the highest standards of operation.
- Cause the patient to accept and effectively Encare disease – their nature long-term, the need is-Guir taking food and so on.
NURSING CARE PLAN
- Reduce inhibited behavior, provide a structured goal-directed activity:
- Spend time with the patient even if it can not respond verbally or do in inconsistently. Direct our concern and care.
- Promise only what you can accomplish realistically.
- Providing the opportunity to learn that their feelings are valid and do not differ much from others
- Limit the patient’s environment to increase their feelings of safety.
- Assign team members to attend the patient therapeutic.
- Start with interactions one by one, and then make progress for the patient to join small groups as tolerated (enter slowly).
- Establish and maintain a daily routine; explain any variation in this patient.
- Increase patient’s self-esteem and feelings of worth:
- Provide care in a sincere way forward.
- Support you in all your successes-enforcement responsibilities within the service, projects, interactions with members of the treatment team and other patients, and so on.
- Helping the patient to improve their appearance help him when necessary torque to shower, get dressed, try washing their clothes, etc..
- Assist the patient to accept greater responsibility for their personal hygiene to the extent that it can do.
- Spend enough time with the patient.
- orient the patient in reality:
- Reorient the patient in person, place and time as needed (call it by name, say the name of the nurse, tell where you are, give the date, etc..).
- Increase the ability of the patient to differentiate between the concept of self and the external environment:
- Helping the patient to distinguish what is real and what is not. Assess the patient’s actual perceptions and sensory perception correct errors in a form that is attached to the facts. Do not argue with the limited validity of patient perceptions nor provide support for them.
- Helping the patient to restore the boundaries of the self:
- Stay with the patient if you are afraid, sometimes touching the patient can be therapeutic. Evaluate the effectiveness of physical contact dcl use in each patient before use consistently.
- Be simple, honest and concise when speaking with the patient.
- Talk with the patient specific issues and simple, avoid ideological or theoretical discussions.
- Direct the activities to help the patient to accept the reality and keep in touch with her, using creative occupational therapy when appropriate.
- Ensuring a safe environment for the patient.
- Reafirmnar the patient that the security environment is explaining the procedures followed in the service, routines, tests, etc., In a brief and simple.
- Protect the patient from self-destructive tendencies (removing objects that could be used in self-destructive behavior).
- Realize that the patient is up actions that are harmful to themselves and others in response to auditory hallucinations.
- 7. – Keep a safe, therapeutic for other patients.
- Remove the patient from the group if their behavior becomes too crowded, annoying or dangerous to others.
- Help the group of patients to accept behavior ‘strange’ patient newcomer simple explanation to the group of patients when necessary (for example, “the patient is very ill at this time, needs our understanding and support”).
- Consider the needs of other patients and plan at least one member of the treatment team is available to other patients if others are needed for patient care newcomer.
- Helping the patient to overcome his regressive behavior.
- Remember: The regression is a purposeful return (conscious or unconscious) to a lower level of functioning-an attempt to eliminate anxiety and restore balance.
- Assess the current level of functioning of the patient and go from that point to your attention.
- Contact the patient’s level of behavior, then try to encourage him to leave his regressive behavior and integrated into adult behavior. Help identify unmet needs or feelings that cause regressive behavior. Encouraging children to express these feelings and help relieve anxiety.
- Establish realistic. Mark the objectives and expectations everyday.
- Ensure that the patient becomes aware of what is expected from him.