Before we go into details of nursing diagnosis for asthma, we should be very aware about what asthma actually is.
Background
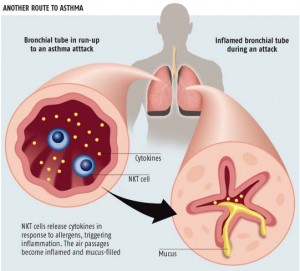
Asthma is a chronic disease requiring lifelong care, which affects the respiratory system. It is an inflammation of the bronchial tubes that carry air to the lungs, due to the irritation caused by certain stimuli such as pollen, pollution, smoke, emotions, laughter, exercise, some medications etc …
This inflammation causes the ducts are more sensitive and responsive to a contraction causing further narrowing. This blockage of air which can be more or less important depending on the sensitivity of the individual, stimulus intensity or how you feel before “contact”, makes the person with asthma has choking, coughing, feeling of pressure chest and wheezing when breathing is important that asthma is well controlled to try to eliminate or reduce the number and intensity of the crisis and pursue a life as normal as possible.
Asthma is a disease of lungs in which an obstructive ventilation disturbance of the respiratory passage. It evokes a sense of shortness of breath. An asthma attack occurs when the respiratory muscles are unable to provide the lungs with air to breathe resulting in short breathing. In the initial stages, the patient can symptoms free for fairly long period of time. As the disease progresses, increasing amount of mucus are secreted in between attacks thus creating an ideal condition for bacterial infection. Bronchial asthma is generally intrinsic, i.e., no cause can be demonstrated for the illness. In some cases though, asthma is caused by specific allergies. Although, allergies are not necessarily the cause of the asthma syndromes.
In sensitive people asthma can be triggered by breathing in allergy causing substances. Common allergens (allergy causing substances) include pets, dust, weather change, change in food habits, exercise, tobacco smokes etc.
Asthma and the Bronchial Tubes
Symptoms can come spontaneously or might be triggered by cold, cold air, tobacco smoke, stress or other pollutants. Generally, the patient breathes normally and has some fits of severe asthma attacks. Asthma can become dangerous if the airway becomes severely restricted. Common symptoms include cough with or without sputum production, pulling of skin between the ribs when breathing and shortness of breath that gets worse with exercise and any other kind of work. Another very common symptom is wheezing that may be worse at night or in the early morning.
When it comes to treating asthma, there are several ways to go about it-inhalers and steroid medications. If the symptoms are acute and severe, a nebulizer is used. We will look into some methods of nursing diagnosis for asthma.
signs/symptoms of Asthma (Must check during The diagnosis):
– persistent coughing
– clearing throat
– difficult breathing, difficulty talking
– audible wheezing
– decreased breath sounds and wheezing by auscultation
– flaring nostrils
– chest retractions
– anxiety, apprehension, panic
– ashen color, circum-oral cyanosis
Assessments
Assessments of asthma should be firstly based on the past medical history of the patient. It is duly required to check whether the patient has any history of asthma or breathing related troubles. It is also necessary to assess the family’s history of any previous lung disease. The patient might not be able to do everything he could earlier. His blood pressure might shoot up and his breath may worsen when the patient lays supine on the bed. The wheezing sounds of breath and chronic coughing might also be signs of asthma. The patient will also have decreased activity rate and lessened libido. Emergency symptoms include bluish color to the face, rapid pulse and sweating.
Treatment information:
For the patient to perform the correct use of treatment should distinguish between and relieving medications that reduce inflammation. know you will have to take daily medication even if you feel well.’ll learn what are the side effects and solutions to reduce patient anxiety. It will tell you what are the guidelines for further treatment. Influence on the positive effects of the medication. We also check the compression of the patient.
Preventive Medication: Anti-inflammatory:
These drugs help prevent or reduce inflammation and congestion of the airways. Therefore, the sensitivity decreases and help prevent attacks. However, do not stop and started an attack. There are two types of anti-inflammatory:
– Corticosteroids: They protect the airways against irritants and allergens. Two routes of administration: Inhaled are commonly used to be administered regularly to be effective. The oral form of pills or syrups, administered for a few days if the airways are very congested.
– No steroids: They protect the airways against allergens. They help prevent attacks caused by exercise. Always administered by inhalation.
Symptomatic medication: Broncho dilators
It works by relaxing the muscles around the airways, widening them and making breathing easier. Bronchodilators There are two types:
– Fast-acting broncho dilators: act quickly to open the airways, making breathing easier quickly, help stop an attack already begun, also help prevent attacks caused by exercise. Are typically administered by inhalation.
– Long-acting broncho dilators: They act more slowly than fast action, but better longer. They can be used regularly. Prevent nocturnal attacks. They also prevent attacks caused by exercise can be inhaled (preferably) or oral.
It is very important to maintain respiration and release broncho constrictions while allowing the mucus plug expulsions. Sudden fits of asthma attacks can also be controlled by control exercises – using diaphragmatic and pulse lip breathing. One of the very important things that need to be stressed is that never leave the patient alone during one of his fits. Reassure the patient as much as you can and place the patient in semi-Fowler position and encourage diaphragmatic breathing. Fowler position allows for easy exchange of gases. Monitor cardiac rate and pulse rate in case of an acute attack and initiate IV access. Educate the patient about potential causes (smoke, allergies, weather changes, etc). Adjust oxygen according to the patient’s vital function and ABG measurements and administer IV fluids to combat dehydration until the patient can tolerate oral fluids, which will help loosen secretions. Encourage the patient to express his fears and concerns about the illness. Also encourage them to identify with one of the care measures. This, in turn, helps promote relaxation.
Correct use of inhalers:
Tubeless inhaler use:
1. – Remove the lid and shake the aerosol.
2. – Pour the air through the nose and mouth.
3. – Hold upright and spray with the nozzle in the bottom.
4. – Put your mouth around the mouthpiece and pressing his lips together, starting to take all the air can slowly through the mouth.
5. – Very beginning to take the air, press the spray once and continue to take air.
6. – Holding your breath for as long as possible (around 10 seconds).
7. – Pour slowly through your mouth.
8. – If you have to do another inhalation wait at least 30 seconds.
Inhaler use with camera:
1. – Join the two parts of the camera by matching the projection of one hand with the other slot.
2. – Remove the lid and shake the aerosol.
3. – Insert the spray nozzle in the area existing for that purpose in the side of the spacer.
4. – Put your mouth around the mouthpiece of the spacer, maintain this horizontal.
5 – Pour some air and press the spray. Then take all the air you can slowly.
6 – Holding your breath for as long as possible (about 10 seconds)
7 – Pour slowly through your mouth.
8 – If you have to do some other inhalation wait at least thirty seconds.
Turbuhaler System:
1 – Unscrew and remove the white cap covering the Turbuhaler.
2 – Hold the inhaler upright with the screw revolving at the bottom.
3 – Load the dose by turning the rotary screw, first to the right and then to the left until it clicks.
4 – Place the mouthpiece between your teeth, close your lips on it and breathe strongly and deeply, hold your breath for 5-10 seconds.
Accuhaler System:
1 – Prepare the dose correctly.
2 – Open the lid which will be discovered the nozzle and move the lever to the other side and you’re ready to shoot.
3 – Place your mouth around the mouthpiece of the device and take all the air that can quickly through the mouth.
5 – Remove the device from your mouth and hold your breath as long as possible (about 10 seconds).
6 – Pour slowly through your mouth.
7 – If you have to do another inhalation wait at least 30 seconds.
Triggers and preventive measures:
Triggers:
1 – Viral infections.
2 – Allergens inhaled: pollens, mites and pets.
3 – Exposure to nonspecific irritants: snuff, smoke, paint odors, perfumes, varnishes, cleaning spray air fresheners and insecticides.
4 – Emotions: laughter, tears, fear, nervousness and stress.
5 – Drugs: aspirin, NSAIDs, beta blockers and others.
6 – Changing weather: cold, heat, storms, rain.
7 – Exercise.
How to avoid triggers:
House dust: mites
The materials they are made of many objects strongly attract dust element where the mites, this is one of the allergens.
You can take simple steps that can reduce the number of dust mites:
1 – Remove dust with a damp cloth or vacuuming. The patient will not enter the room during cleaning.
2 – Clean filters, heat and air conditioning at least once a month.
3 – Avoid carpets, rugs and upholstered chairs.
4 – Avoid toys or plushies, ensuring that they are wooden or allergenic.
5 – The curtains should be washable cotton or plastic.
6 – Avoid comforters or pillows or wool and used foam pillows and duvets acrylic fabric.
7 – linen or flax or pajamas.
8 – Do not store or knitting wool blankets in the closet.
9 – The bedding should be washed with water at 60 º C.
10 – Reducing moisture at least 50%.
11 – Do not wear slippers or lined leather gloves.
Pollen:
1 – During the pollen season and avoid mowing lawns and gardens take the field.
2 – Keep windows and doors closed.
3 – Avoid having plants to flourish.
4 – Do not ride a motorcycle, bicycle and car with the windows closed it.
5 – Avoid the exits to the street in pollination peak hours and use sunglasses and mask.
6 – Before bedtime moisten the atmosphere of the room.
Pets:
1 – Keep animals away.
2 – Wash dogs and cats once a week.
3 – Avoid approaching them.
Fungi:
1 – Avoid stains in the house.
2 – ventilate and clean with bleach kitchen and bathroom.
3 – Save to making sure the laundry is dry.
4 – Leave your shoes or sneakers out of the room.
Exposure to nonspecific irritants:
1 – Do not smoke and avoid smoking in places where you are asthmatic.
2 – Do not use air fresheners or insecticide spray.
3 – Avoid scented wipes and perfumes.
4 – Do not use talcum powder.
5 – Avoid the presence of asthma in places where there are paints, varnishes and solvents.
6 – Do not use cleaning products that give off a great smell like ammonia or strong water,
7 – Avoid presence of smoke and fume extractors use.
Infections:
1 – Vaccinations.
2 – Hygiene measures.
3 – Avoid contact with infected people.
Maximum expiratory flow measurements:
We explained that the way to know when it’s right and when you start a crisis is by the presence of discomfort and this is an objective need to know and use and maximum expiratory flow meter. We teach measurement and found that the right way has learned the technique.
The FME is the speed at which you can blow air out of the lungs with one breath.
Rules for use of maximum expiratory flow meter.
1 – Set the display to zero.
2 – standing or sitting up straight.
3 – Hold the meter horizontal to the ground without clogging the exhaust.
4 – Put the mouthpiece in your mouth closed lips meter around.
5 – Blow forcefully and more quickly than you can. Remove the meter from his mouth.
6 – The marker will have moved on the scale, remember the number and put the marker back to zero.
7 – Repeat the test two more times and record the highest number of the three in his diary or chart.
We hope That the nursing diagnosis for asthma is more understandable now – Just follow the guidelines.